MRI Scans and Transient Ischemic Attack (Mini-Strokes): Timeliness Makes a Difference
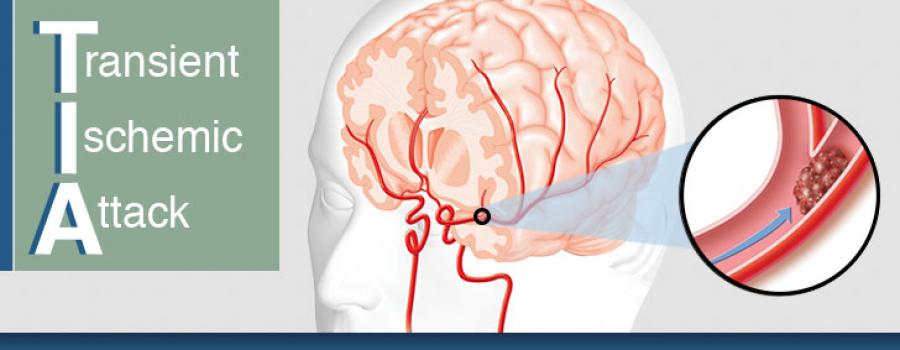
A transient ischemic attack (TIA) or commonly referred to as a mini-stroke has traditionally been regarded as a minor and temporary condition, but timely MRIs have proven that these events belong on the same spectrum as strokes. However, because TIAs, by definition, only last a short time, MR imaging must take place as quickly as possible for the fullest yield of useful information.
There is now a consensus that having a TIA increases a person’s risk of a stroke.
Approximately one in six people who survive a TIA suffer a stroke within 90 days. Undergoing an MRI as soon as possible after a TIA can detect crucial warning signs that computed tomography (CT) alone cannot see.
Previous consensus guidelines from the American Heart Association (AHA) do not recommend MRI for all TIA patients because of the higher cost. However, mounting evidence suggests that an MRI within 1 to 2 days of a TIA could spot evidence of a stroke that may disappear in time.
MRIs can detect tissue damage even when symptoms are temporary.
The sophisticated imaging technique can detect stroke lesions that may become less apparent quickly. A study from the journal Stroke followed 263 patients who had suffered a TIA or minor stroke and received a baseline MRI within 24 hours. After 90 days, a follow-up MRI was conducted.
The results of each patient’s two MRIs were assessed independently and the results confirm the importance of early scans. Thirty percent of patients with a negative scan at 90 days had a clearly identifiable stroke in the baseline image. Without the early scan, physicians would not know that a stroke had occurred in this large group of patients.
In spite of this evidence, some physicians settle for a less-precise CT scan. A recent study from Neurology found that just 40 percent of patients with TIA or minor stroke had an MRI performed within 48 hours.
New guidelines offer options for those at high-risk of stroke.
The AHA and American Stroke Association have published new consensus guidelines for preventing strokes in patients with a history of strokes or TIA. Reducing hypertension and statin therapy remain at the top of the list. Increasing physical activity, reducing sodium intake, and following a Mediterranean-style diet (as opposed to a low-fat diet) are recommended. Other practices, such as sleep assessments and anti-platelet therapy immediately following a TIA may be considered.
For patients with a history of stroke or TIA, the average annual rate of future stroke is at an all-time low. That’s great news, but a more nuanced understanding of TIAs and timely MRI of those who suffer them could yield even more impressive results.
References:
AHA and ASA Release Guideline for Prevention of Future Stroke in Patients with Stroke or TIA. American Family Physician. January 2015;91(2):136-137. Available from: https://www.aafp.org/afp/2015/0115/p136.html
Chaturvedi S et al. Have clinicians adopted the use of brain MRI for patients with TIA and minor stroke? Neurology. January 2017;88(3):237-244. doi:10.1212/WNL.0000000000003503
Krieger D. Should patients with TIAs be hospitalized? Cleveland Clinic Journal of Medicine. August 2005;72(8):722-724. Available from: http://www.clevelandclinicmeded.com/medicalpubs/ccjm/august2005/krieger.htm
Moreau F et al. Early Magnetic Resonance Imaging in Transient Ischemic Attack and Minor Stroke: Do it or Lose it. Stroke. March 2013;44(3)671-674. doi:10.1161/STROKEAHA.111.680033