The Power of MRI Exams in Personal Injury Lawsuits
The health and wellbeing of individuals are often vulnerable to mishaps and accidents that can cause personal injuries. Such injuries could result in a legal dispute where the injured person, known as the plaintiff, seeks compensation for damages from the person or entity they believe caused their injury. In these instances, a comprehensive understanding of the injury's extent is paramount, often heavily relying on medical records and procedures. One such crucial diagnostic tool is the Magnetic Resonance Imaging (MRI) examination. This article delves into how MRI exams can provide substantial assistance in personal injury lawsuits.
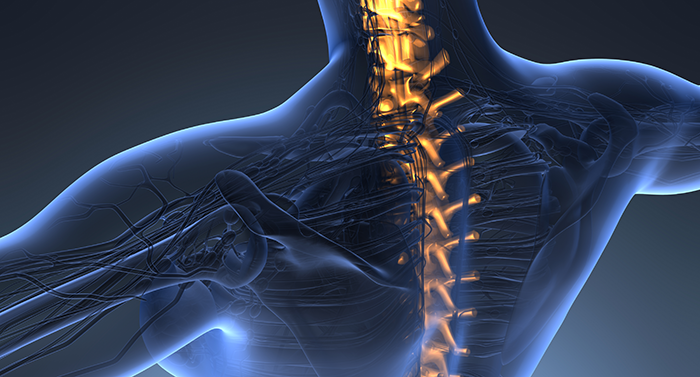
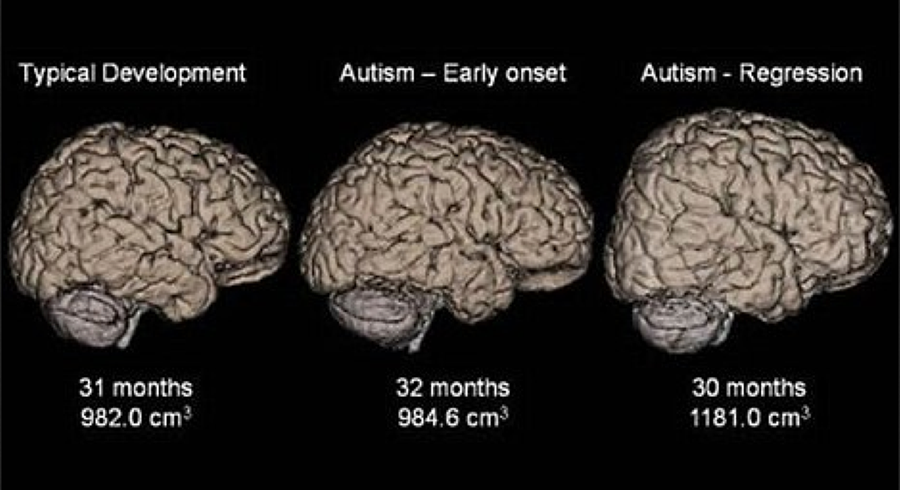
MRI is a non-invasive imaging technique that employs a powerful magnetic field and radio waves to generate detailed images of the inside of a body, typically focusing on soft tissues and organs. Unlike other imaging techniques like X-ray and CT scans, which primarily concentrate on skeletal injuries, MRI scans provide a comprehensive view of non-bony structures, like muscles, ligaments, tendons, and even the brain. This ability to visualize soft tissues makes MRI a valuable tool in evaluating the full extent of an injury.
In the context of personal injury lawsuits, MRI scans serve multiple critical roles. Primarily, it provides an objective basis for the plaintiff's claims of injury. Subjective symptoms like pain, discomfort, or restricted mobility may not convince a jury. However, visual evidence of damage, such as a torn ligament or herniated disc, becomes a tangible piece of evidence supporting the plaintiff's claims. By demonstrating the injury's existence and severity, MRI results can counter any argument that the plaintiff is exaggerating or feigning their condition.
Secondly, MRI results can contribute to determining the prognosis of an injury. The extent of damage revealed in the scan can help predict the duration of recovery, potential complications, and the possibility of permanent disability. This information is crucial in estimating the future medical costs, loss of earnings, and even non-economic damages like pain and suffering, which the plaintiff may include in their claim for compensation.
Furthermore, the timing of an MRI can also be a strategic element in a personal injury case. Early MRI exams might not reveal certain types of injuries like soft tissue damage, as these can take time to manifest. An MRI performed too soon could lead to an underestimation of the injury's extent, possibly harming the plaintiff's case. On the other hand, an MRI conducted too late might give the defendant an opportunity to argue that the injury was caused by something other than the initial incident. Hence, the timing of MRI is a critical factor in personal injury cases.
Finally, it's important to note that MRI results need to be interpreted and presented by a medical expert. Precise Imaging has several board certified radiologist that will review the images taken by the technologist and provide a report with their finding.
In conclusion, MRI examinations can be a powerful tool in personal injury lawsuits, aiding in confirming the existence and severity of an injury, predicting its prognosis, justifying medical expenses, and providing compelling evidence for the jury. However, these benefits are maximized when the timing of the MRI and interpretation of its results are strategically managed. It's crucial for individuals in these situations to consult with both medical and legal professionals to ensure the most effective use of MRI examinations in their case.